- Non Specific Spinal Pain
- Facet Joint pain
- Discogenic Pain
- Sacroiliac Joint Pain
- Sacroiliac Joint Pain Mediated Through Pelvic Instability
Non-Specific Mechanical Pain
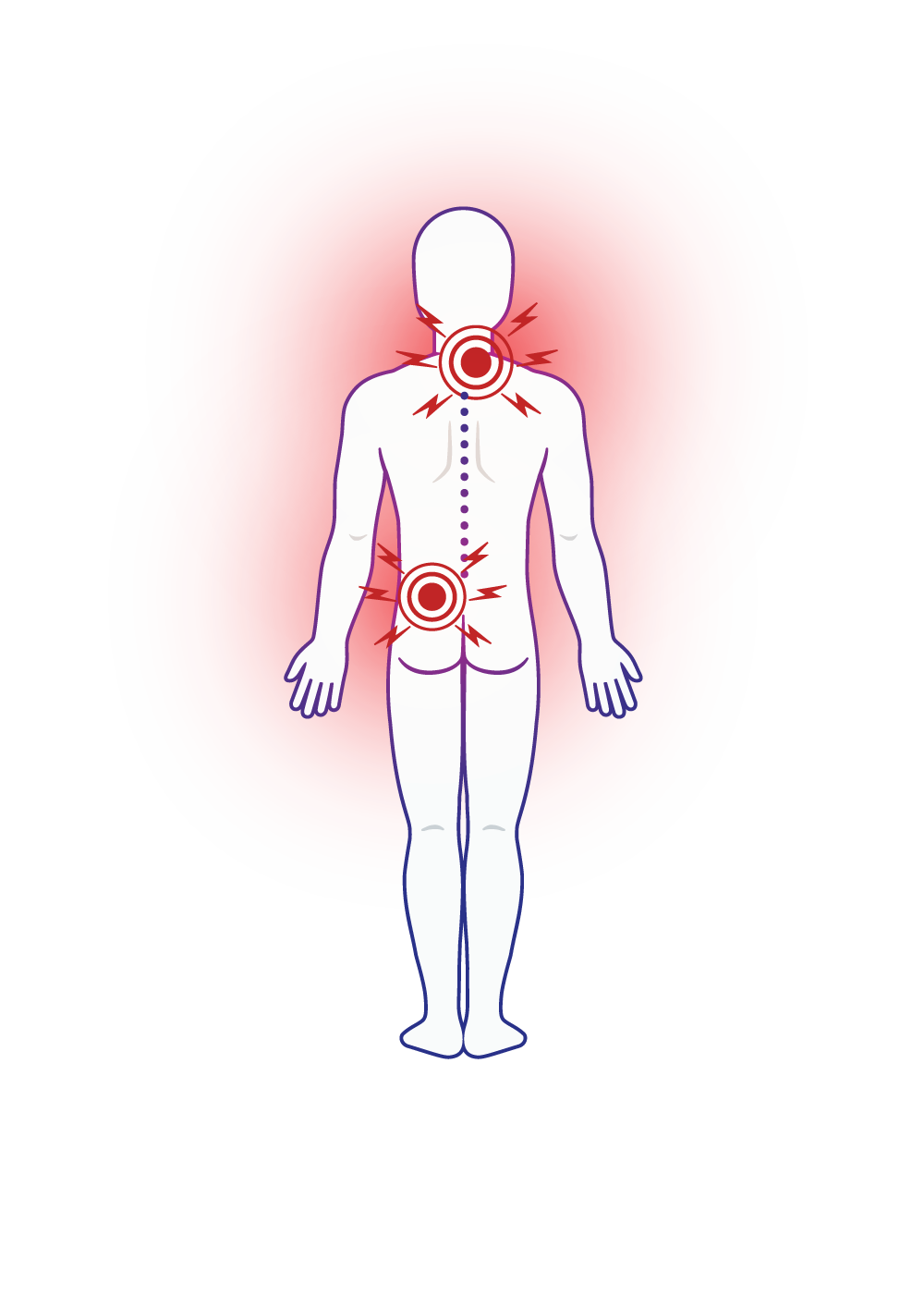
Spine pain – lower back and neck pain, is very common. Most of us will experience spine pain at least once every year. Most of these pain presentations are benign and usually resolve within a few days. The cause varies from acute muscle and soft tissue injuries to joint and disc injuries.
During these acute pain presentations, it is important to keep moving, even gentle movement is OK. Try to find a position or movement that you can do and tolerate and build on that – even if it hurts a bit. Physiotherapy and other physical therapies can be helpful to release muscle spasms and to get you going again. Pharmacological measures including paracetamol, anti-inflammatories, and low dose neuroleptic medication (Amitriptyline) can be taken for a short period of time.
It is only if spine pain persists that we consider a specific structural cause for the pain. The most likely causes for persistent mechanical spine pain are facet joints and discs in the neck and back, as well as sacroiliac joints in the lower back.
Facet Joint Pain
Overview
There are 24 vertebrae that stack on top of each other to form your spinal column. At the back of each vertebrae are 2 facet joints that connect one vertebrae to the next. Facet joints contribute to spinal stability and mobility. Each facet joint has a capsule and the joint surfaces are covered with cartilage.
Symptoms
When a facet joint is damaged or inflamed it can cause local spine pain over the area of the joint. The nerve associated with the joint can also produce pain. You might experience that as back, buttock or leg pain –which could travel all the way down to your foot.
The pain sometimes goes down my leg –how does that come from the back?
Referred pain is caused by one part of your body but felt in another. Referred facet joint pain can be sharp and severe at times in the back, where it is felt most strongly. It tends to be duller in the leg. Nerve pain tends to concentrate more in the leg and has a thinner, shooting quality.
What Causes Facet Joint Pain?
Facet joint injuries commonly occur in association with trauma, especially twisting and hyperextension type injuries. Facet joints are commonly affected by osteoarthritis (especially in older people) that causes degeneration of the cartilage of the joint surfaces.
Do I need to get a scan to show my facet joint injury?
We will decide whether you need scans based on the unique features of your presentation. We urge caution with SPECT nuclear medicine scans and MRI for facet joint pain because of the high false-positive rates. These scans may detect an abnormality (most of us have a few oddities) which is not necessarily causing the pain/a problem.
Diagnosis
Localised pain on spine extension and rotation may indicate facet joint pain. Diagnosing facet joint pain is complicated because X-rays, CT scans, bone scans and MRIs cannot establish whether a facet joint is the source of pain. The most reliable way to diagnose facet joint pain involves using a guided anaesthetic injection into either the joint or its nerve supply (medial branch block). If the injection temporarily makes the pain go away, it’s a good indication that the problem is in your facet joint.
Treatment
Facet joint pain can present as an acute attack, which eases quickly, or can build up over time and last longer. It’s not always possible for your doctor to confidently predict what will happen in the long term. However, in our experience, many patients recover well.
Is there any proven treatment?
Treatments such as hands-on physiotherapy and exercise-based therapy are helpful in some cases but can often be employed more effectively once underlying pain is reduced. Intra-articular facet joint corticosteroid injections can be helpful for a short period of time. The only treatment proven to work for facet joint pain is radiofrequency neurotomy that targets the nerve supply to the joint. Unlike the hip, knee and shoulder joints, there is so far no facet joint replacement available.
Discogenic Pain
OVERVIEW
The disc is the strong mobile structure that forms the major connection between each of your vertebrae. While many disc injuries will heal naturally and pain will subside, the most common cause of chronic low back pain does originate from discs. It is considered that discs become painful because of once-off or repetitive trauma. Specifically, lifting and twisting stresses can lead to disc injury. These stresses may cause the bony plate between the disc and the vertebra to crack. This then leads to a weakening of the disc. A radial tear may then occur in the outer part of the disc. It is then possible for the soft, internal part of the disc (the nucleus) to spread along the radial tear into the outer part of the disc. This material is highly irritating when it comes into contact with the small nerves in the outer part of the disc. Recent studies have shown the vertebral end plate to be the main pain mediator for discogenic back pain. Once a tear reaches the nerves in the outer part of the disc, pain symptoms will commence.
Symptoms
The nature of the pain is usually deep and aching. It can spread to the legs and groin as well. However, pain in the back will be worse than the leg pain. When pain spreads from the disc into the leg, the pain is known as referred pain. The pain that may be felt down the leg is not sciatica, as is sometimes thought, although sciatica can occur if disc material irritates or compresses spinal nerves. In the case of discogenic pain, the sciatic nerve is not being pinched or aggravated. Rather, the pain is referred from inside the disc itself. Severe discomfort in a sitting position is often the most incapacitating symptom of discogenic pain. Patients with pain originating from the disc also have problems standing and generally feel best when moving about. However, these aggravating features also occur with other causes of back pain, so no assumptions can be made before proper diagnosis has been reached.
Diagnosis
Examinations by your doctor may produce varied results. The strange thing about discogenic pain is that the spinal range of movement can be normal and straight leg raise tests also normal. There may be localised tenderness. Plain x-rays are unhelpful. Likewise, CT does not offer any further diagnostic value. These tests can be used to exclude other causes of back pain, but MRI is the best preliminary test. The most common finding on MRI is degeneration, which occurs in all people eventually. Disc changes on MRI scans are, on most occasions, not helpful to make a diagnosis of discogenic back pain, however when there are Modic type I and to a lesser extend Modic type II vertebral endplate changes visible on MRI, research has shown a high correlation with discogenic lower back pain from that disc level.
The most accurate test for discogenic pain is a procedure called a provocative discography.
Treatment
There is no proven treatment for discogenic pain. It is advisable to exercise despite this pain and progressively return to normal movements and activities. Treatment options, should the pain persist, include surgery (discectomy with disc replacement or spinal fusion).
Exciting new treatments that target the nerve supply to the vertebral end plate (basivertebral nerve) can provide pain relief in patients with vertebral endplate mediated pain. Intra-disc therapies such as PRP (platelet rich plasma), which are still experimental, can help to improve discogenic back pain. Other treatment options include neuromodulation or nerve stimulation to improve spinal stability through activation of the multifidus muscles.
Sacroiliac Joint (SIJ) Pain
Overview
The sacroiliac joints are large, strong fibrous joints between the sacrum and the ilium bones of the pelvis. They are connected by strong ligaments. The sacroiliac joints connect the spine to the pelvic and hip girdle. The sacrum supports the spine and in turn, is supported by an ilium on each side. The inner surfaces of these joints are irregular and incongruous. This, along with the complex arrangement of strong posterior ligaments, and compression of the joint by deep core muscles, aids the stability of the joints. Sacroiliac joint pain is thought to arise from chronic inflammation or irritation within the joint, capsule and/or deep ligaments that support the joint (the deep interosseous & long dorsal ligaments), which form the posterior capsule. This irritation may arise from excess movement of the joint, inflammatory arthritis, or damage from trauma.
Symptoms
If due to trauma, sacroiliac joint pain is mostly unilateral, otherwise it may be bilateral. Features of sacroiliac joint pain are non-specific. That is, they often mimic symptoms typical of pain caused by lumbar facet joints, hip joints and discs. However, the presence of prominent pain over the sacroiliac joint is present in 80% of people with primary sacroiliac joint pain.
Sacroiliac pain is classically deep and aching in character and may refer with a deep, dull, ache across the buttocks and into the lower legs. Referred pain from the sacroiliac joint and ligaments can reach the foot. A history of a fall onto the buttocks is common. Sacroiliac joint pain pattern is predominantly in the buttock, but can also refer to the thigh, the groin and the leg.
Diagnosis
Many physical examination tests are used to diagnose sacroiliac joint pain. However, when tested against the gold-standard of intra-articular injection, they have been shown to be inaccurate. X-rays and scans of this joint are generally unhelpful in diagnosing it as a source of pain. The only imaging test that has any real validity is a ‘bone scan’.This scan, however, has very low sensitivity in picking up sacroiliac joint pain, and therefore is not generally warranted.
The best method to diagnose sacroiliac joint pain is an image guided injection into the joint with local anaesthetic, followed by substantial eradication of pain in the immediate post-injection period.
Treatment
An injection into the intra-articular and ligamentous component of the joint with local anaesthetic and a corticosteroid can provide relief for a short period of time. Radiofrequency denervation of the lateral branches of the spinal nerves that innervate the joint can provide long-term relief in sacroiliac joint pain.
Sacroiliac Joint Pain mediated through Pelvic instability
Overview
Pelvic instability can present at any age, but tends to decline with aging, due to stiffening of ligamentous tissues. Our pelvic bones bear the weight of our upper body and distribute it through the hips and legs. The pelvis consists of the hip, sacrum and pubic bones all held together by ligaments. If ligaments are injured or overstretched, the pelvis loses its stability and begins to move excessively with physical activities.
It often presents in young females who are involved in sport that requires a high degree of mobility (such as dance or gymnastics). It can also present during pregnancy or post-partum, as the hormone, relaxin (which relaxes the pelvic ligaments in preparation for childbirth) is still circulating in the system. There may be a history of injury that causes the pain. Often pain will commence insidiously and be associated with prolonged postures rather than moving or physical activity.
The underlying cause of pain is deformation of structures in the spine and pelvis (joint and ligaments) due to excessive range of motion without the necessary muscular control. The joints are held at or near their end range of motion, which stresses and stretches the retaining ligaments.
Symptoms
Symptoms include pain in the sacroiliac joints, lower lumbar spine and pubic region. There may be radiation of pain to the groin or hip. Pain when rolling over in bed, climbing stairs, getting dressed, and getting out of the bath are highly suggestive of the condition.
Diagnosis
A physical examination and a series of provocative tests (physical manoeuvres) are used to diagnose pelvic instability. A pelvic support belt or brace may provide significant relief and point to instability. Special investigations like MRI scans are usually unhelpful to make a diagnosis of pelvic instability pain. An immediate significant reduction in pain after sacroiliac joint injection can help to confirm the diagnosis.
Treatment
Pelvic instability pain is managed by a multi-disciplinary team focussing on physical therapies to improve pelvis stability through deep pelvic muscle activation, psychological support, and interventions.
Interventions aim to improve pelvic stability and treat the pain. Prolotherapy treatment involves injecting a 50% glucose solution among the stabilising ligaments of the sacroiliac joints and symphysis pubis to create an inflammatory reaction and hence scarring of the ligaments which, in turn, will improve stability. Pulsed radiofrequency stimulation of the ligaments can help to reduce nerve sensitivity pain from the ligaments.